Thrombosis
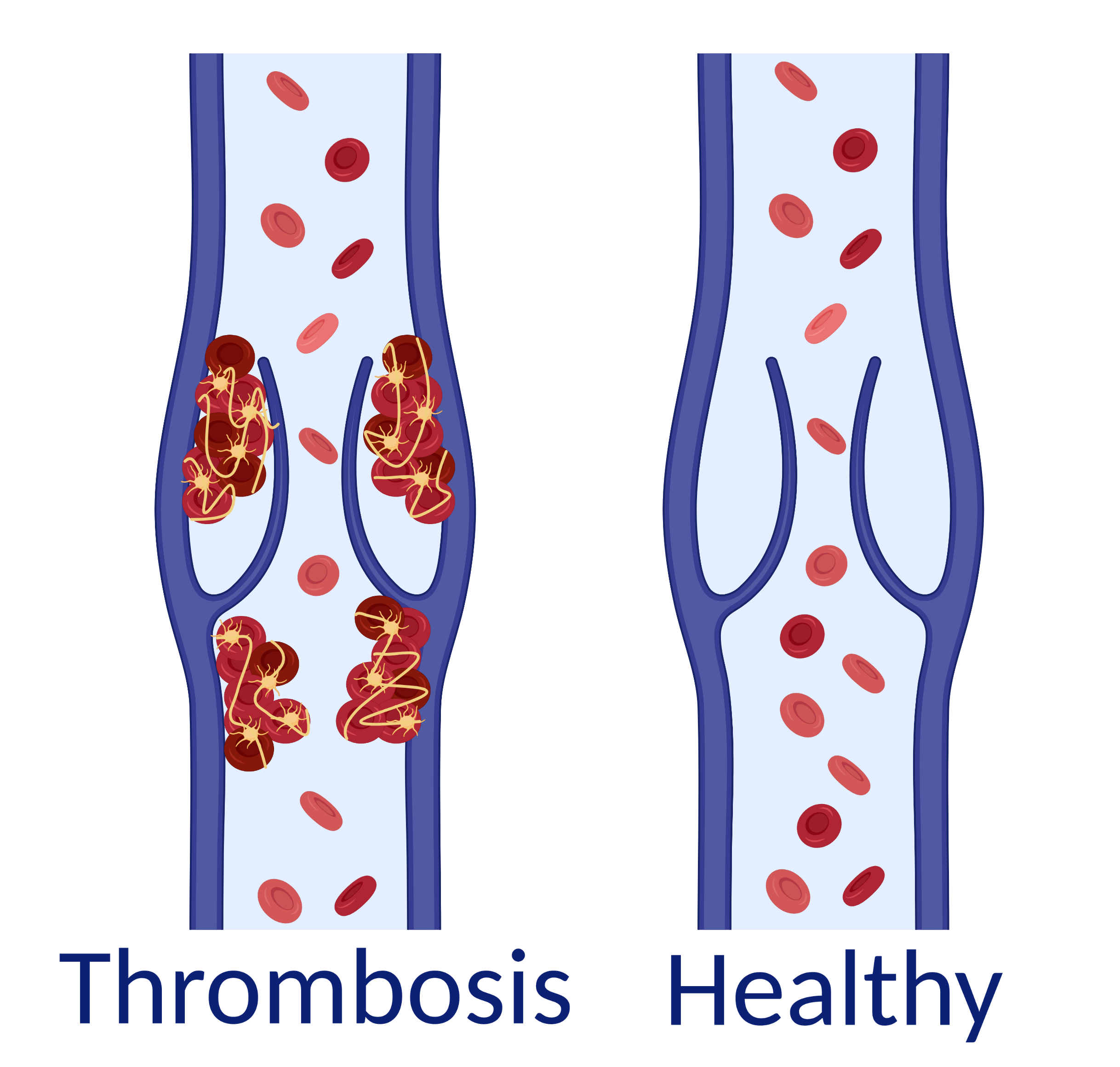
Thrombosis occurs when a blood clot forms in a blood vessel and the blood no longer flows properly. Thrombosis can develop in a vein or an artery.
When a thrombosis blocks a vein, we call it venous thrombosis. This thrombosis is usually in the leg or abdominal cavity. When the clot breaks off, it can get stuck in the small vessels in the lungs. This blockage is called pulmonary embolism. If the clot forms in the lungs, it is also called pulmonary embolism. Thrombosis in the large, deep veins in the legs is called deep vein thrombosis (DVT).
When a thrombosis blocks an artery, it is called arterial thrombosis. If the clot breaks off and gets stuck in the heart or small vessels in the brain, it can cause a heart attack or a stroke.
Thrombosis in a vein
Thrombosis in a vein
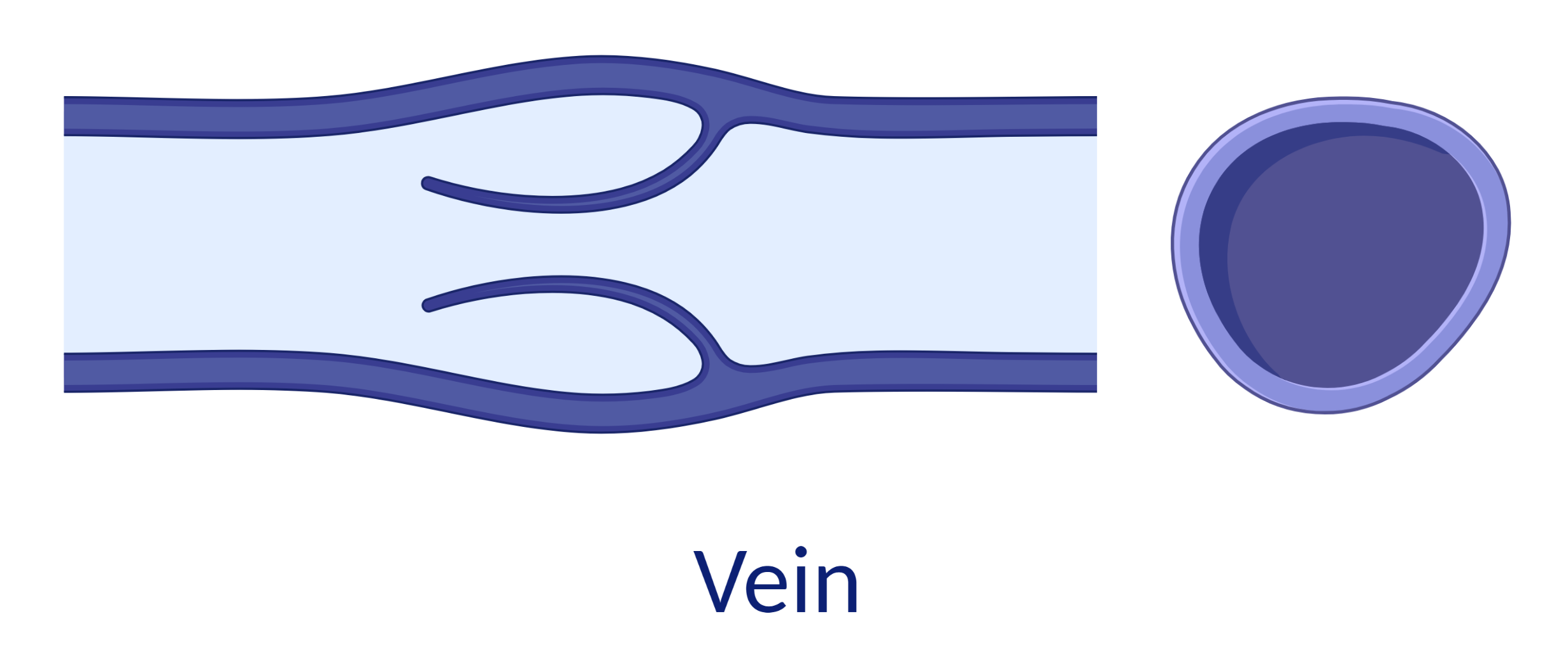
Veins are blood vessels that return blood from the body to the heart. Veins have thin walls and valves that keep blood from flowing in the wrong direction.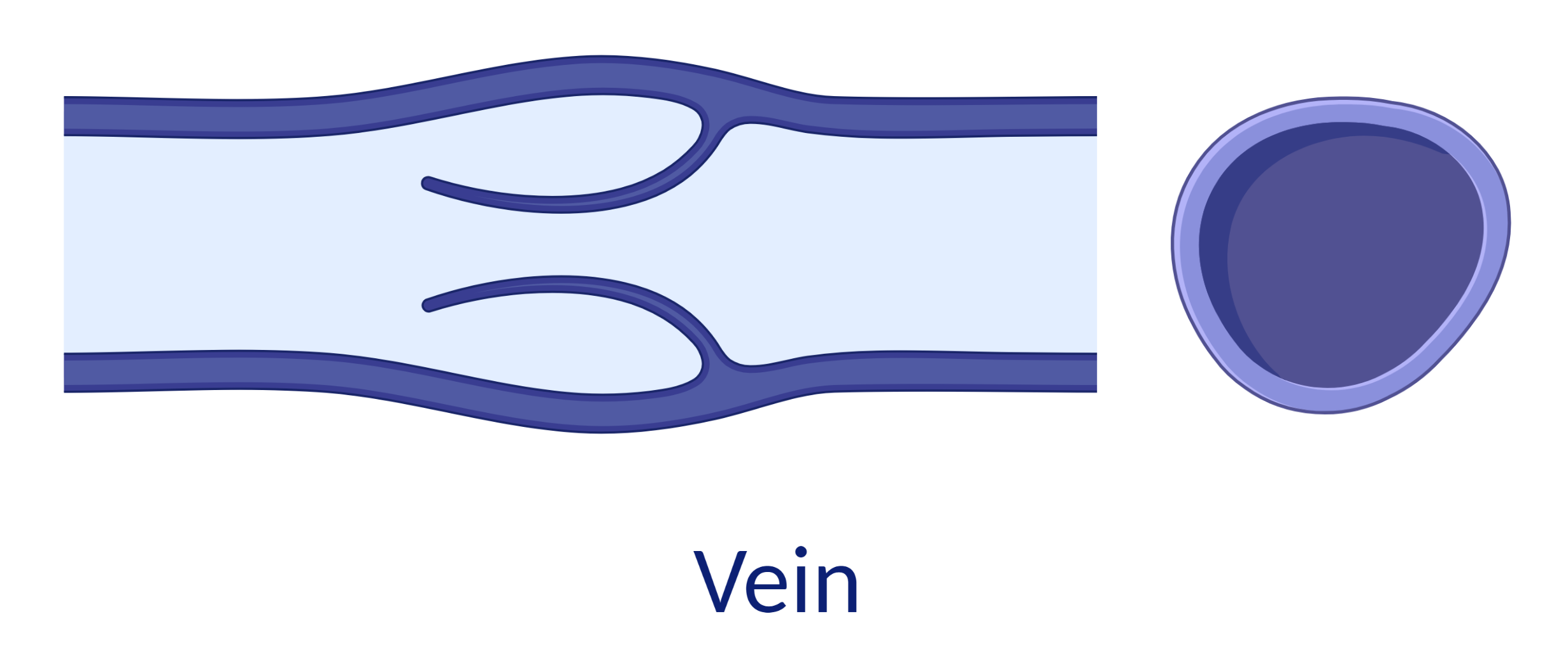
When a thrombosis blocks a vein, we call it venous thrombosis. This thrombosis is usually in the leg or abdominal cavity. When the clot breaks off, it can get stuck in the small vessels in the lungs. This blockage is called pulmonary embolism. If the clot forms in the lungs, it is also called pulmonary embolism. Thrombosis in the large, deep veins in the legs is called deep vein thrombosis (DVT).
Thrombosis in an artery
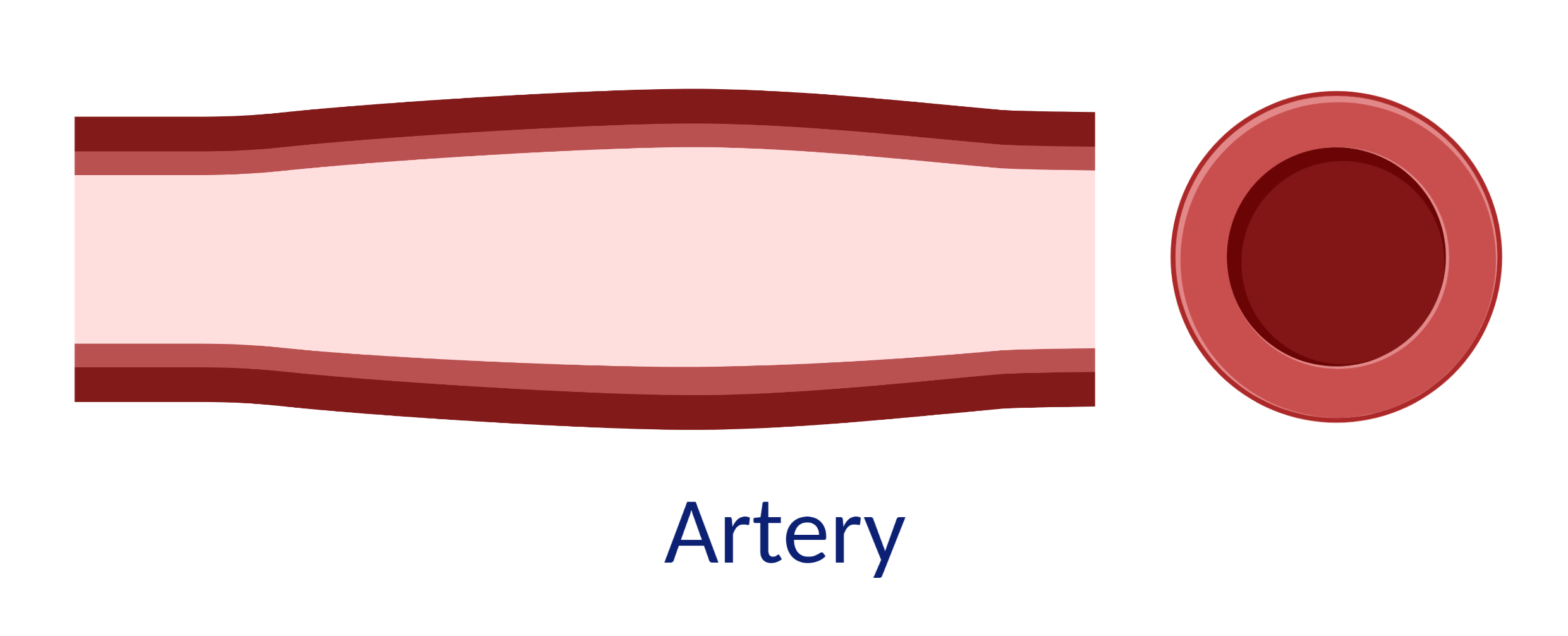
Arteries are blood vessels that carry blood from the heart throughout the body. These arteries have a thick, elastic wall. Blood flows quickly in the arteries.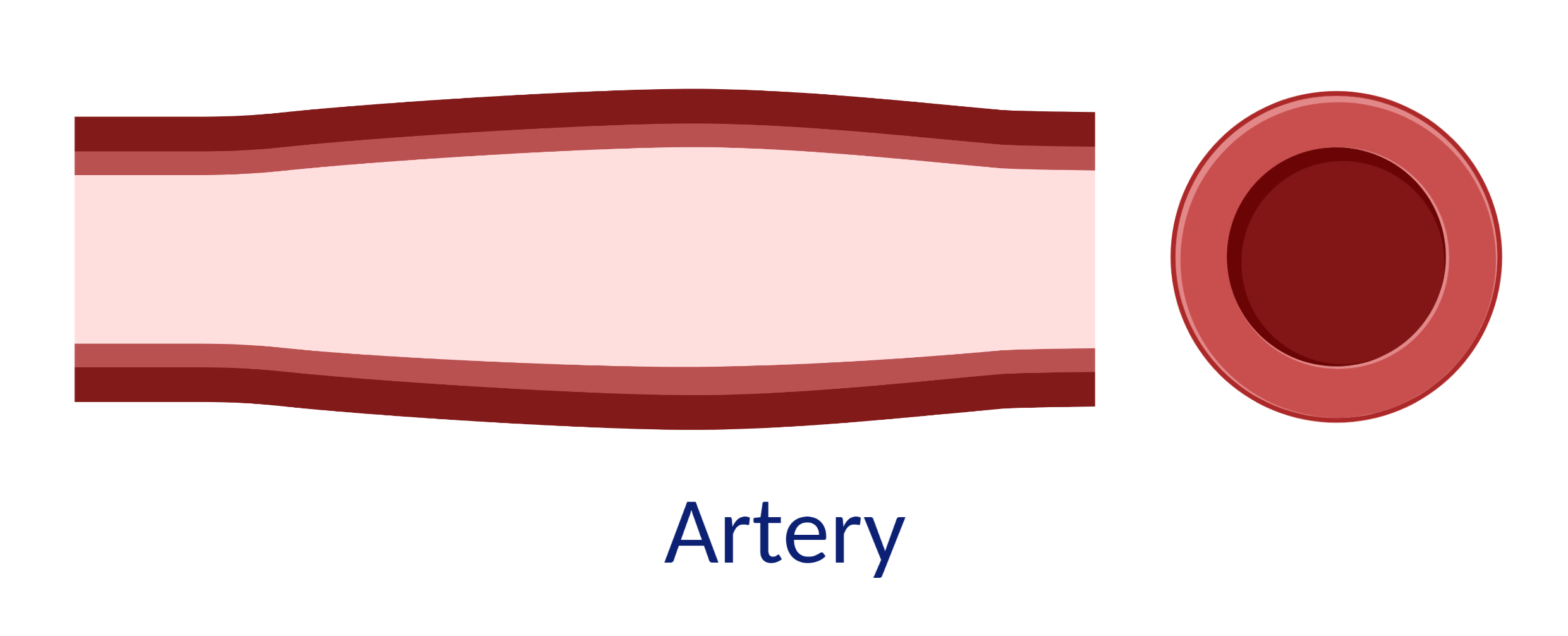
When a thrombosis blocks an artery, it is called arterial thrombosis. If the clot breaks off and gets stuck in the heart or small vessels in the brain, it can cause a heart attack or a stroke.
How does thrombosis occur?
Thrombosis can arise when your clotting system is out of balance. Our blood contains substances that make your blood clot if you have a wound. The body forms a clot that stops the bleeding. Once the bleeding has stopped, the clot breaks down again. When this system is out of balance, it can cause a clot to form in places where it is not needed.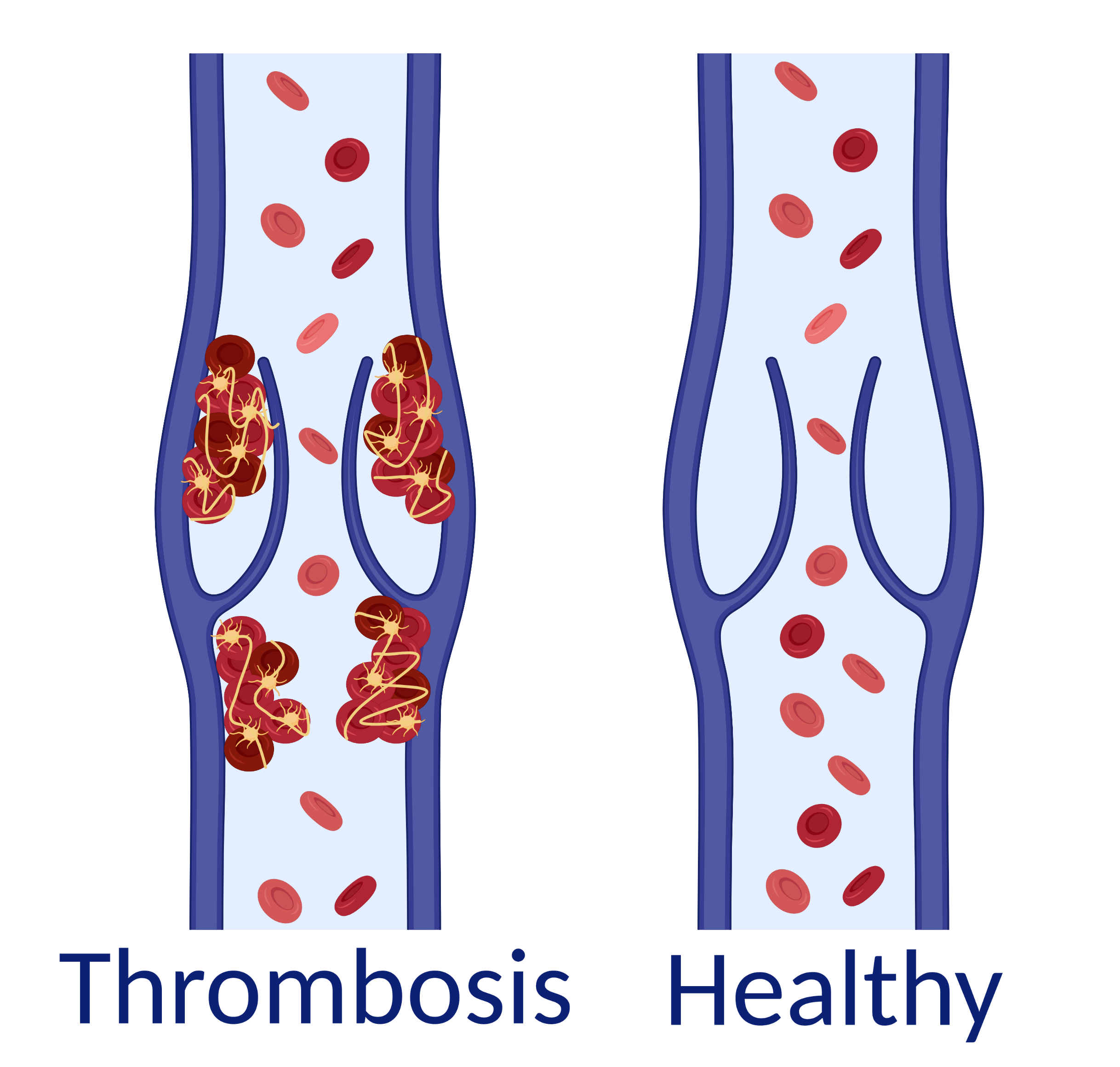
Thrombosis in a vein
Anticoagulants
Anticoagulants, commonly called blood thinners, are medicines that help prevent blood clots. This reduces the chance of you developing thrombosis.
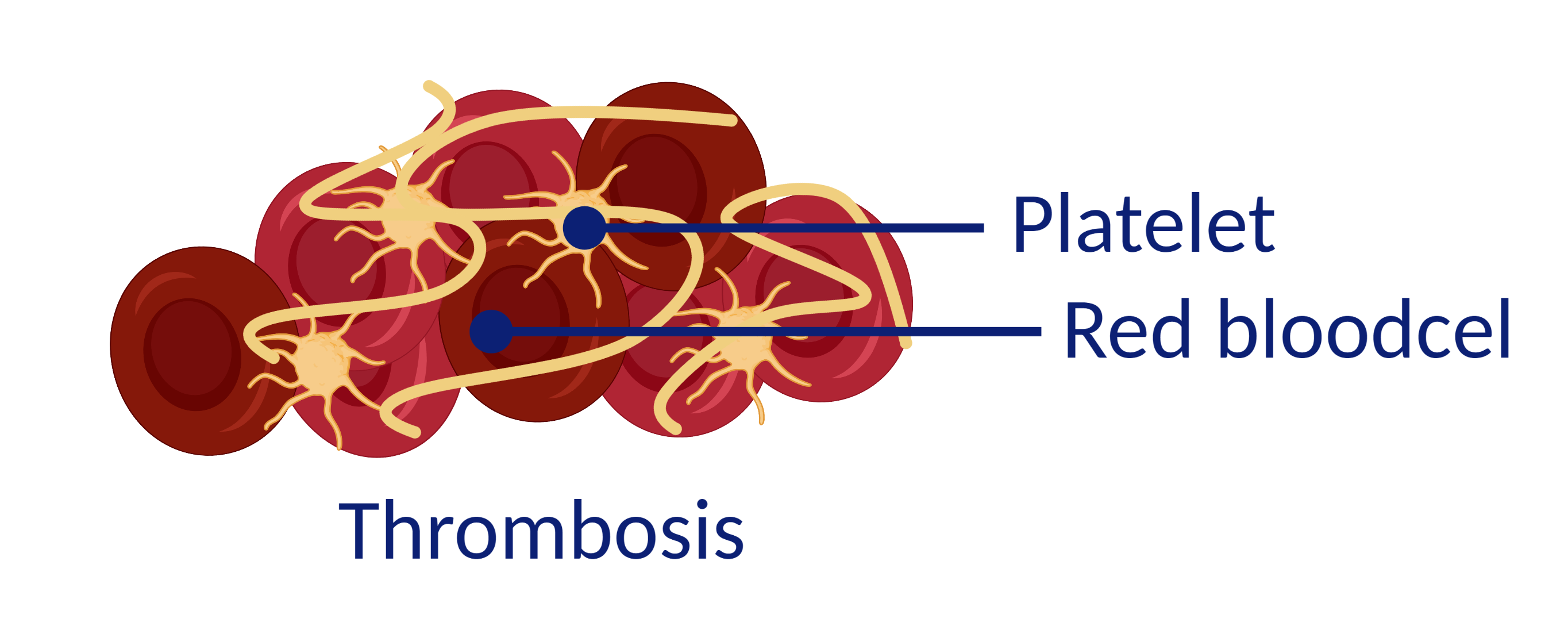
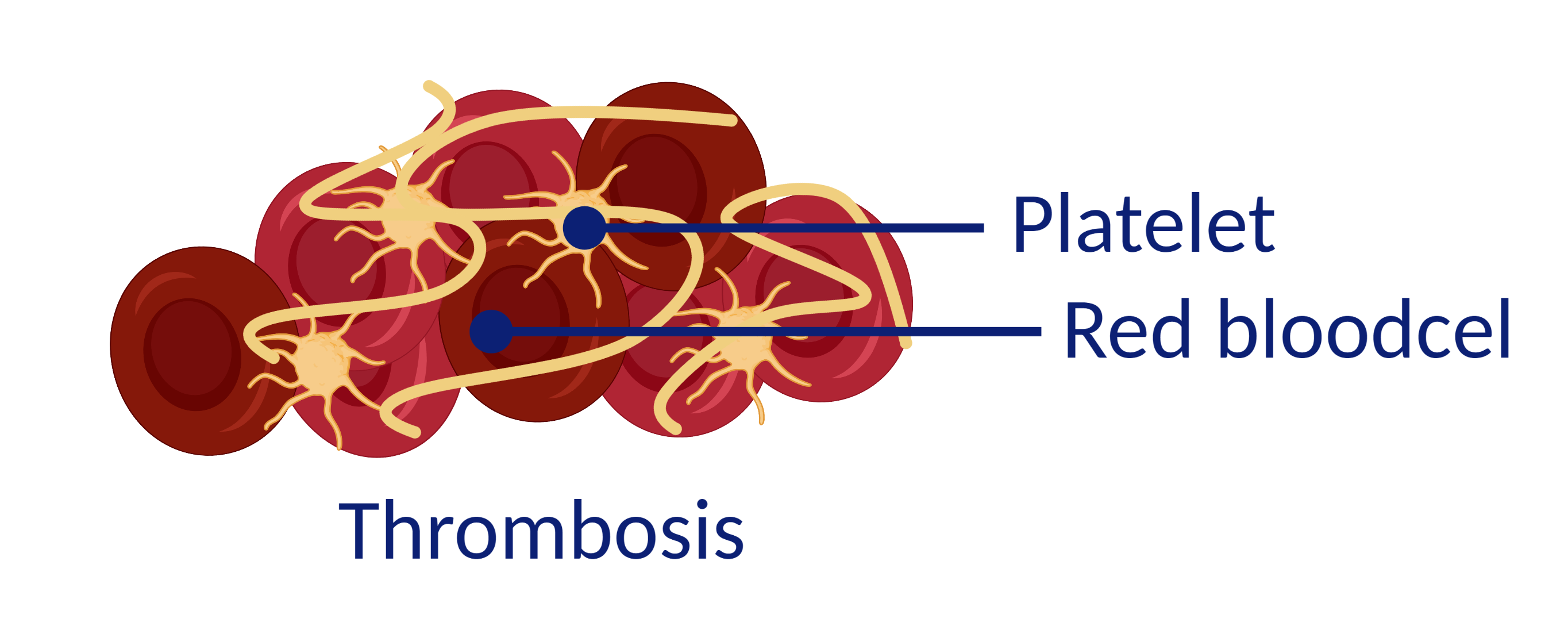
Platelet inhibitors or platelet aggregation inhibitors
Platelets are small cells that stick together to form a clot. The inhibitors make the platelets less sticky so that a clot is less likely to form.
This medicine is often used for (a risk of) thrombosis in the arteries. They are considered 'light' blood thinners that are (relatively) easy to use. The inhibitors come in tablet form and are usually given in one dose. You do not need to have your blood checked.
Vitamine K antagonists (VKA)
Vitamin K is a substance that your liver uses to make clotting factors. By inhibiting vitamin K, fewer clotting substances will be produced. As a result, your blood will clot less quickly.
VKAs are often used in the case of artificial valves, atrial fibrillation and thrombosis. VKAs are tablets. It is difficult to determine how many VKAs you need. If you take these tablets, your blood can clot too slowly or too quickly, for example, due to illness, a different diet or changes to your medication. That is why, if you take VKAs, you will be registered with the thrombosis service. The thrombosis service will check your blood regularly. The amount of VKAs you can take is determined based on the values in your blood.
The thrombosis service is always available for questions about VKAs.
Direct Oral Anticoagulation (DOAC)
DOACs stop the action of one specific clotting factor.
DOACs are used in the case of thrombosis legs, pulmonary embolism and to prevent thrombosis in atrial fibrillation. DOACs are tablets. These tablets work as well as VKAs. DOACs have a stable effect and are (relatively) easy to use. Blood clotting doesn't go too slowly or too quickly, which means there is no need to monitor your blood with DOACs. You take a fixed dose every day as prescribed by the doctor.
DOACs have a short effect and quickly disappear from your body. If you forget to take the tablets, the risk of thrombosis increases.
It is, therefore, important that you remember to take your tablets.
Low Molecular Weight Heparins (LMWH)
Low Molecular Weight Heparins are anticoagulants in the form of injections. You can inject these syringes (or have them injected) under your skin. Your doctor will determine the dose (amount) of the LMWH based on your kidney function, weight and the reason you are taking blood thinners.
The LMWH injections are prescribed if you:
When will you be given anticoagulants?
The risk of thrombosis is higher with various diseases and specific procedures or surgeries. We give you anticoagulants to reduce the chance that you will get thrombosis (again). We prescribe anticoagulants for these diseases, procedures and surgeries:- A heart rhythm disorder, such as atrial fibrillation (arrhythmia).
- An artificial heart valve.
- After angioplasty or stent placement.
- After thrombosis.
- After a stroke or heart attack.
- After surgery or while wearing a plaster cast; when you are less mobile.
- A hereditary clotting disease.
- Cancer, especially during treatment.
Types of anticoagulants
There are four types of anticoagulants. Your doctor will determine which medicine is best for you.Platelet inhibitors or platelet aggregation inhibitors
Platelets are small cells that stick together to form a clot. The inhibitors make the platelets less sticky so that a clot is less likely to form.
This medicine is often used for (a risk of) thrombosis in the arteries. They are considered 'light' blood thinners that are (relatively) easy to use. The inhibitors come in tablet form and are usually given in one dose. You do not need to have your blood checked.
Vitamine K antagonists (VKA)
Vitamin K is a substance that your liver uses to make clotting factors. By inhibiting vitamin K, fewer clotting substances will be produced. As a result, your blood will clot less quickly.
VKAs are often used in the case of artificial valves, atrial fibrillation and thrombosis. VKAs are tablets. It is difficult to determine how many VKAs you need. If you take these tablets, your blood can clot too slowly or too quickly, for example, due to illness, a different diet or changes to your medication. That is why, if you take VKAs, you will be registered with the thrombosis service. The thrombosis service will check your blood regularly. The amount of VKAs you can take is determined based on the values in your blood.
The thrombosis service is always available for questions about VKAs.
Direct Oral Anticoagulation (DOAC)
DOACs stop the action of one specific clotting factor.
DOACs are used in the case of thrombosis legs, pulmonary embolism and to prevent thrombosis in atrial fibrillation. DOACs are tablets. These tablets work as well as VKAs. DOACs have a stable effect and are (relatively) easy to use. Blood clotting doesn't go too slowly or too quickly, which means there is no need to monitor your blood with DOACs. You take a fixed dose every day as prescribed by the doctor.
DOACs have a short effect and quickly disappear from your body. If you forget to take the tablets, the risk of thrombosis increases.
It is, therefore, important that you remember to take your tablets.
Low Molecular Weight Heparins (LMWH)
Low Molecular Weight Heparins are anticoagulants in the form of injections. You can inject these syringes (or have them injected) under your skin. Your doctor will determine the dose (amount) of the LMWH based on your kidney function, weight and the reason you are taking blood thinners.
The LMWH injections are prescribed if you:
- Need to have surgery.
- Have a period of bed rest.
- Are pregnant and have venous thrombosis or an increased risk of thrombosis.
- Are not yet stable enough on the tablets from the thrombosis service after thrombosis or pulmonary embolism.
- Have to temporarily stop your anticoagulants because of surgery or a (dental) procedure (we call this bridging).
What to watch out for when taking anticoagulants
Anticoagulants make your blood clot less quickly which reduces the risk of thrombosis. The slower blood clotting also makes you bleed more easily, and a wound (on the outside or inside of your body) will bleed for longer and more heavily.
You must take the anticoagulant properly and follow the doctor's advice. Otherwise, the medicine can be dangerous. If your blood clotting is too slow, it can be very difficult to stop the bleeding. Pay attention to bleeding warning signs.
You must take the anticoagulant properly and follow the doctor's advice. Otherwise, the medicine can be dangerous. If your blood clotting is too slow, it can be very difficult to stop the bleeding. Pay attention to bleeding warning signs.
Bleeding warning signs
Contact your treating specialist, general practitioner or the thrombosis service (if they are monitoring you) immediately if you have:- Red-coloured urine.
- Black stools or blood in your stools.
- Loss of feeling in an arm or leg, a drooping face or cannot speak properly.
- Sudden, severe pain in the abdomen.
- A large bruise of more than 10 cm in diameter.
- Sudden onset of bruising with no apparent cause.
- A prolonged nosebleed that lasts for more than half an hour.
- Coughing up or vomiting blood.
In combination with other medicines
Some medicines can affect how anticoagulants work by enhancing or counteracting the effect. Your pharmacy, your attending physician and the thrombosis service must have an up-to-date overview of all of the medicines you are taking. This also applies to medicines that you buy without a prescription. Always make sure you have an up-to-date medication overview with you if requested.Surgery and procedures with anticoagulants
If you have to undergo a procedure, dental treatment or surgery during your anticoagulant treatment, please tell your treating doctor and anaesthetist that you are taking anticoagulants. For some procedures, it may be necessary to stop your anticoagulant medication for a while to prevent bleeding. If you are being treated by the thrombosis service, you must let them know that you are having a procedure or surgery. They need to know what surgery you are having and when it will take place.Lifestyle rules with anticoagulants
It is important to always take the anticoagulant medicines as prescribed. If you forget a dose, consult the thrombosis service or pharmacist about what to do.

We do not recommend doing certain sports that increase the risk of bleeding. Because you take anticoagulants, you bleed for longer, and it is less easy to stop bleeding. The sports we advise against are:
Be alert
Please remain alert while taking anticoagulants. If you are going home from the hospital or going to a care home, make sure your anticoagulant medication does not change. Always tell your doctor or nurse that you are taking anticoagulants when you are discharged.
Exercise and sports
Sports and exercise are always good. Exercise lowers blood pressure and reduces the risk of thrombosis. It also reduces the risk of osteoporosis.We do not recommend doing certain sports that increase the risk of bleeding. Because you take anticoagulants, you bleed for longer, and it is less easy to stop bleeding. The sports we advise against are:
- Contact sports such as (kick) boxing and judo.
- Scuba diving and mountaineering above 2500 metres.
Holidays
Always make sure you have enough medicine with you for the duration of your trip. Take an up-to-date medication list with you; in English if possible. You can request this from the thrombosis service or the pharmacy. If anything happens on holiday, tell the emergency workers that you are taking anticoagulant medicines and show them the medicine list.More information
The Thrombosis Foundation Netherlands
Dobbeweg 1A, 2254 AC Voorschoten
Telephone: (071) 561 77 17
Website: www.trombosestichting.nl
E-mail: tsn@trombosestichting.nl
You can also request a free personal Anticoagulant Card from the Thrombosis Foundation Netherlands.
Other important information:
De Harteraad
Prinses Christina- Amaliastraat 10, 2496 XD Den Haag
Telephone: (088) 111 16 00
Website: www.harteraad.nl
Federation of Dutch Thrombosis Services (FNT)
Rijnsburgerweg 10, 2333 AA Leiden
Telephone: (071) 561 77 76
Website: www.fnt.nl
E-mail: fnt@fnt.nl
More information about anticoagulants on thuisarts.nl (in dutch):
Ik gebruik een bloedverdunner (DOAC). Waar moet ik op letten?
Ik gebruik een bloedverdunner (cumarine). Waar moet ik op letten?
Ik gebruik een bloedverdunner (bloedplaatjesremmer). Waar moet ik op letten?
Ik ben vergeten mijn bloedverdunner te slikken
Dobbeweg 1A, 2254 AC Voorschoten
Telephone: (071) 561 77 17
Website: www.trombosestichting.nl
E-mail: tsn@trombosestichting.nl
You can also request a free personal Anticoagulant Card from the Thrombosis Foundation Netherlands.
Other important information:
De Harteraad
Prinses Christina- Amaliastraat 10, 2496 XD Den Haag
Telephone: (088) 111 16 00
Website: www.harteraad.nl
Federation of Dutch Thrombosis Services (FNT)
Rijnsburgerweg 10, 2333 AA Leiden
Telephone: (071) 561 77 76
Website: www.fnt.nl
E-mail: fnt@fnt.nl
More information about anticoagulants on thuisarts.nl (in dutch):
Ik gebruik een bloedverdunner (DOAC). Waar moet ik op letten?
Ik gebruik een bloedverdunner (cumarine). Waar moet ik op letten?
Ik gebruik een bloedverdunner (bloedplaatjesremmer). Waar moet ik op letten?
Ik ben vergeten mijn bloedverdunner te slikken
Heeft u nog vragen?
If you have any questions, ask your doctor or general practitioner, the thrombosis service or pharmacist.

This information was made in collaboration with Beter Keten. This is a partnership between various hospitals in the Rotterdam Rijnmond region.
This information was made in collaboration with Beter Keten. This is a partnership between various hospitals in the Rotterdam Rijnmond region.