Research agenda 2021-2025
Introduction
The burden of cancer
Cancer affects all of us – even if we do not get diagnosed with the disease we will inevitably see a family member, friend or someone else close to us suffer. As the population grows older, more and more patients will be diagnosed with cancer each year. Whereas cancer often still is an acute and life-threatening disease, it becomes a chronic disease for some patients. This comes not only with tremendous personal impact, but with enormous societal costs as well, in the form of lost healthy life years and growing healthcare costs. We, at the Erasmus MC Cancer Institute, have committed our careers to combat cancer on a regional, national, and international level by providing excellent care, groundbreaking research, and optimal screening and prevention. Our goal is that less people develop cancer, and to improve the lives of those who do, providing personalized treatment where possible and alleviating symptoms when cure is beyond reach.
Who are we?
The Erasmus MC Cancer Institute unites scientists and health professionals from 15 departments within the University Medical Center Rotterdam, all involved in cancer care, education and research. The Cancer Institute facilitates cross-fertilization between researchers working on cancer-related topics and physicians who participate in often multidisciplinary cancer teams.
The integration of clinical care, teaching and research on one tight-knit campus – one of our unique selling points – in the heart of Rotterdam stimulates this process by creating a melting pot of care, education, and science. These oncology-focused ‘living labs’ optimize cross talk and synergy to develop, validate and implement new diagnostic and therapeutic technologies swiftly. Close collaboration with Delft University of Technology (TU Delft) and Erasmus University Rotterdam fuels medical-technological innovations and their implementation even further.
Research is key
Research has a pivotal role in our mission. Cancer is not one specific disease, but an extremely heterogeneous collection of conditions. It can manifest itself in almost all parts of the body. It affects many older patients, but can occur at very young age as well. Some tumors respond very well to specific treatments, while other tumors – even of the same type – do not respond at all. To provide the best care for each patient we need to understand what is going on: in the cells – what happens before cancer sets on?; in the tumor – what drives its growth and spread?; in the patient – when and how can we treat most optimally?; in our healthcare system - how can we improve its efficiency and quality? Our commitment to improve the lives of patients is driven by our curiosity to understand cancer in all its aspects and our shared responsibility to provide both optimal and affordable care.
Why a research agenda?
A research agenda identifies priorities and outlines a framework for future research activities. Articulating a research agenda improves the focus and quality of cancer related research. Finally, a research agenda helps to make visible what we do and why we do it – for science and for society.
Research agenda
Exploiting creative tensions
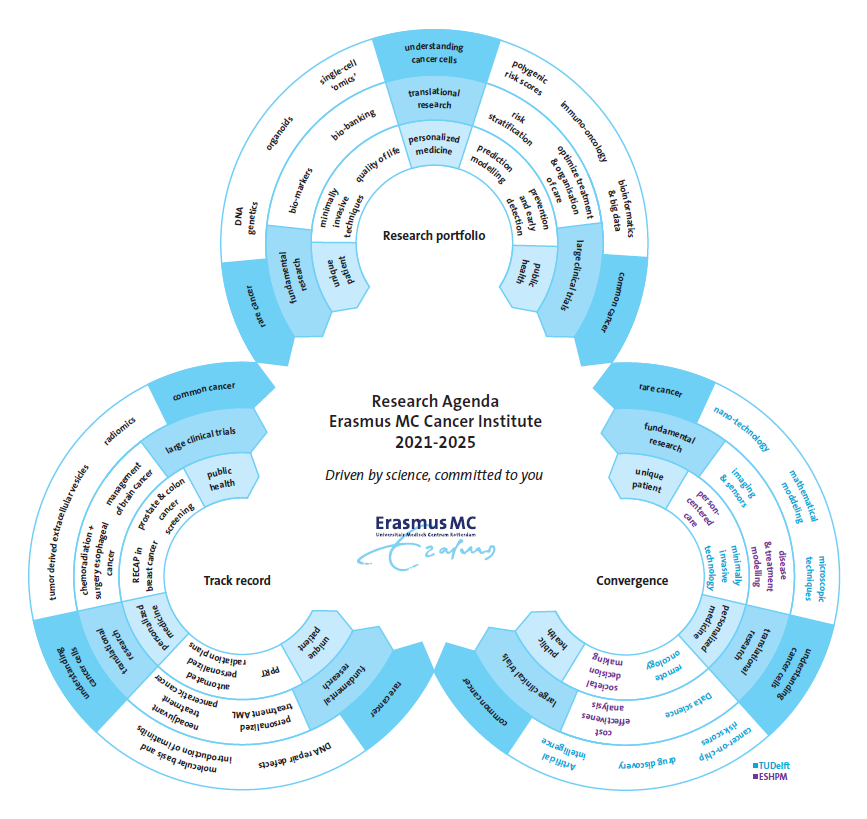
Our research agenda addresses the whole cancer control continuum, and includes topics such as the characterization and understanding of cancer cells at a molecular level, new, often noninvasive, diagnostics and treatment strategies, the identification of risk factors, optimizing patient stratification, and includes rare and common cancers for all ages. This broad but interconnected range of research topics reflects the unique position of the Erasmus MC, connecting all clinical specialisms and research approaches on one campus. It also provides us with a paradigm for the organization of our oncological research: not in isolated academic groups but in interdisciplinary centers where ‘lab’ and ‘clinic’ collaborate intensively.Within this continuum, three ‘tension arcs’ can be discerned, on which our key research activities can be located. These tension arcs connect seemingly contrasting concepts that can be considered either the beginning or the end of the continuum: from first principles to complex cases, from laboratory science to implementation, and from the individual patient to public health.
Vision, results, collaborations
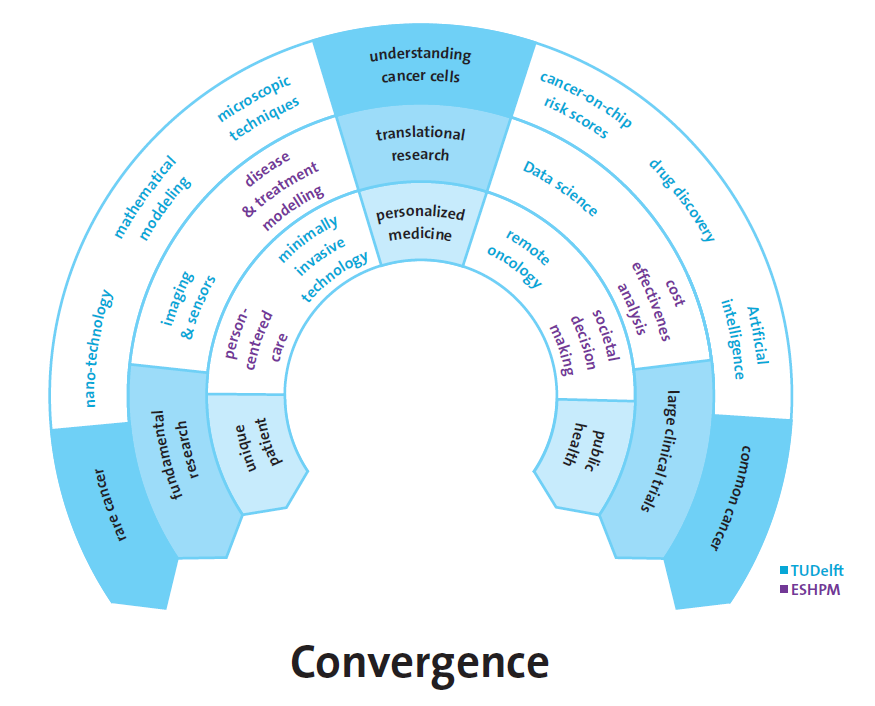
These three arcs are used to map our current research vision, our track record in oncology, and our collaborations with TU Delft and EUR. In the next sections, the tension arcs that are the backbone of our research agenda will therefore be used to map: (1) the research topics and areas which we will pursue, (2) inspiring results from the last decade, to illustrate how these arcs are a creative driving force behind our research, and (3) the intensive, converging collaborations with our nearby partners at the Erasmus University Rotterdam and Delft University of Technology.Creative tensions I: research vision
The figure below depicts the tension arcs structuring the continuum of our research activities. Each arc represents a dimension on which our research activities can be mapped: 1) from very rare cancers to very common cancers, 2) from fundamental laboratory research to large international clinical trials, 3) from the unique, individual patient to society at large. It is our research vision to exploit the productive tensions that arise along these arcs to gain new scientific insights into onset, development and treatment of cancer, to provide better care for cancer patients, and to contribute to a society where cancer is adequately screened for, where each cancer patient receives optimal treatment, and where cancer care remains cost-effective.
Tension arc 1: from first principles to complex cases
This arc describes how a focus on understanding rare cancers and cancer predisposition syndromes, derived from single (epi)-genomic alterations, provides insights that go beyond elucidating that specific cancer and vice versa. The acquired molecular mechanistic knowledge can be applied to common cancers with complex genetic make-up. Conversely, dissecting complex cancers provides insight into fundamental (epi)genetic mechanisms common to virtually all forms of cancer.
Tension arc 2: from laboratory science to clinical implementation
This arc shows the synergy between fundamental laboratory science, large investigator initiated clinical trials and health technology assessment for societal decision making. On the one hand we aim to rapidly translate key findings from our fundamental science towards clinical implementation. On the other hand, the large, relatively homogenous cohorts of patients involved in large clinical trials provide very detailed and structured information about treatment response and are a rich source of tissue samples which are investigated in depth in the basic science laboratories.
Tension arc 3: from the individual patient to public health
This arc starts from the fact that every individual is unique with respect to his/her concerns, risk profile and preference for and response to treatment. Yet at the level of society as a whole, we can all be assigned to large groups with common traits. Extrapolating the concept of ‘the unique patient’ to society can improve care pathways and investigating large populations may shed light on specific subgroups within the population that warrant more study. This in turn can lead to an improved organization of the health care system, that ultimately benefits individual patients as well.

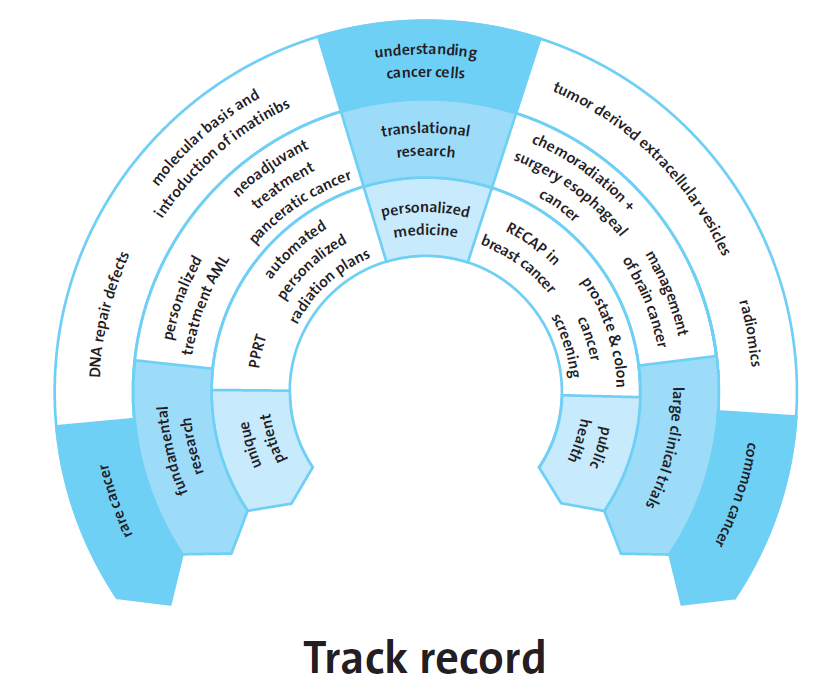
Creative tensions II: results
We publish over 900 cancer related scientific papers and around 30 of our PhD students defend their thesis successfully annually. In addition to increased understanding of cancer in its different forms, many of our findings also find applications in the clinic, to improve the treatment of cancer. The figure below maps a few of our key findings in the last decade on the tension arcs, to emphasize the feasibility of the current research goals of the Erasmus MC Cancer Institute. These achievements, listed below, are examples of major scientific breakthroughs, often with global impact, that increased the understanding of cancer and changed the way we care for our patients.
- The Erasmus MC Cancer Institute lead the world largest trial in pancreatic cancer, which showed that neoadjuvant treatment is superior.
- We changed the standard of care for esophageal cancers from surgery alone to chemoradiotherapy and surgery.
- We played a major role in the detection of tumor derived extracellular vesicles that helps us to understand the development of cancer and may function as biomarkers for patients.
- Erasmus MC Cancer Institute stood at the cradle of prostate and colon cancer national screening programs using simulation modeling followed by large clinical trials.
- In women with breast cancer, we demonstrated that breast conserving surgery was the best choice of
treatment from a cost-effectiveness perspective, wherein both patient reported outcomes and societal impact are taken into account. - We head large international trials in acute myeloid leukemia (AML) testing personalized treatment approaches. Moreover, the biobank linked to these trials resulted in an increased understanding of blood stem cells and their role in hematological malignancies.
- After discovering the role of DNA repair defects in cancer, new cancer treatments were introduced and the RECAP test was developed to select cancer patients for precision therapy.
- Sophisticated radiotherapy treatment planning software was developed and implemented that automatically generates the best radiation treatment plans for patients, increasing the quality of care and decreasing costs simultaneously.
- The data generated in large international clinical trials lead by investigators from the Erasmus MC Cancer Institute has improved the diagnosis, treatment choice, and prognosis of patients with brain cancer globally.
- Using machine learning and artificial intelligence, radiological images can be used as non-invasive diagnostics (‘radiomics’) and replace biopsies of cancers that are difficult to reach, such as brain cancer biopsies.
- We provided the molecular basis of the very successful introduction of the first precision cancer drug in the world: Gleevec (imatinib), in patients with chronic myeloid leukemia and Gastro-Intestinal Stroma Tumors.
- We have improved peptide receptor radionuclide therapy and introduced 177Lu-Luthera, the first FDA and EMA approved peptide receptor radionuclide therapy (PRRT), to combat neuroendocrine tumors
Creative tensions III: convergence
To realize our ambition to provide excellent care, perform groundbreaking research, and to optimally screen and prevent cancer, we collaborate with many partners – regional, national and international, academic research groups, hospitals, companies, and patient advocacy groups, to name just a few. With two academic partners we collaborate in an increasingly intensive manner: the Erasmus University Rotterdam (EUR) and with Delft University of Technology (TU Delft). The Rotterdam-Delft Convergence collaboration is key in the ambition to become the first technical university medical center in the Netherlands. A few examples of key collaboration projects with these two partners are listed below and mapped on the tension arcs below.
- Remote oncology investigates the possibilities for remote follow-up and monitoring for cancer patients. Patients are supported with self-management information, have access to test results, telemedicine applications and technical innovations to monitor their health status and treatment response.
- Societal decision making aims to develop a fair and sustainable societal decision and drug pricing model, taking into account the interest of industry, patients, professionals and society.
- Minimal invasive technologies not only reduce the burden of diagnostic and treatment monitoring (e.g. by optic guided surgery), but also allow us to gain new insights, such as into formation of metastases (by liquid biopsies).
- Person-centric care takes the person’s unique set of circumstances into consideration to offer the best possible care for each person.
- Artificial intelligence and data science can be used to develop prediction models for (radiological) image analysis and optimal personalized radiotherapy.
- Nano-technology studies the smallest molecules and atoms to improve our understanding of cancer development and progression and its response to treatment.
- Cancer-on-a-chip is a culture of a patient’s tumor and is a powerful tool to better understand cancer cells and predicts the response to treatments without exposing the patient.
- Holland Proton Therapy Center’s mission is to find the value of proton therapy and ways to improve its efficacy and cost effectivity through fundamental and clinical research embedded in a global network.
- Mathematical modeling is pivotal. Bioinformaticians model data derived from single cancer cells and health economists model cancer patients’ journeys and their response to treatments.
- Organisation of care is changing rapidly. New technologies such as virtual and augmented reality, speech translation, clinical decision support systems are now available or under development to support the interaction between patient and physician in ‘consultation room 2030’ or during surgical procedures in operating theatres.